What Is Pco2? The Essential Marker of Respiratory and Metabolic Balance Revealed
What Is Pco2? The Essential Marker of Respiratory and Metabolic Balance Revealed
Pco2, or partial pressure of carbon dioxide, is a critical physiological parameter that measures the concentration of dissolved CO₂ in blood—specifically in arterial blood—and serves as a cornerstone for assessing respiratory function, acid-base equilibrium, and overall metabolic stability. Backed by decades of clinical research, Pco2 reflects the efficiency with which the lungs exhale carbon dioxide, a waste product of cellular metabolism and the primary driver of respiratory regulation. Understanding Pco2 is essential not only for intensivists and emergency physicians but also for clinicians managing chronic diseases, anesthesiologists, and researchers studying metabolic pathways.
At the biochemical level, carbon dioxide plays a dual role: it is both a byproduct and a regulator. When cells generate energy, carbon atoms from nutrients convert into CO₂, which dissolves in blood plasma and forms bicarbonate (HCO₃⁻) via the carbonic anhydrase reaction. This transformation keeps blood pH tightly regulated, with deviations signaling potential acidosis or alkalosis.
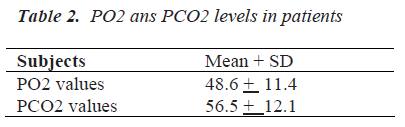
Pco2 is the direct indicator of how well this balance is maintained, making it an immediate and responsive signal of physiological stress. Normally, arterial Pco2 ranges between 35 and 45 millimeters of mercury (mmHg), though minor variations occur based on age, sex, altitude, and metabolic rate. Deviations outside this range demand clinical attention, as even small shifts can impair oxygen delivery and neural function.
Pco2 and Respiratory Physiology: The Breath-Holding Pulse of Carbon Dioxide
Respiration’s central purpose extends beyond oxygen exchange—it is the primary mechanism for eliminating CO₂.Each breath modulates Pco2, creating dynamic fluctuations that trigger automatic respiratory responses. Central and peripheral chemoreceptors monitor Pco2 levels in cerebrospinal fluid and arterial blood, adjusting respiratory rate and depth accordingly. When Pco2 rises—such as during exercise or in airway obstruction—the brainstem stimulates deeper, faster breathing to expel excess gas and restore homeostasis.
Conversely, suppressed respiratory drive, as seen in sedation or neuromuscular disease, leads to CO₂ retention, causing blood acidification.
Clinical measurement of Pco2 typically relies on blood gas analysis, a routine test in intensive care units that provides real-time data on acid-base status. Non-invasive methods, such as capnography, continuously track exhaled Pco2 during anesthesia or respiratory support, offering immediate feedback on ventilation efficacy.
For example, during mechanical ventilation, maintaining an end-tidal Pco2 (EtCO₂) of 35–45 mmHg ensures adequate gas exchange without over- or under-ventilation. In chronic obstructive pulmonary disease (COPD), patients often develop “CO₂ retention” due to impaired alveolar ventilation; their stable Pco2 reflects long-term compensation, underscoring the parameter’s diagnostic value.
Metabolic Implications: When Pco2 Speaks Beyond Respiration
Though Pco2 is fundamentally a respiratory gauge, its fluctuations frequently signal metabolic disturbances. In states of reduced tissue perfusion, like shock, anaerobic metabolism accelerates, flooding blood with lactate and temporarily suppressing CO₂ elimination—producing paradoxical “compensated” acid-base shifts.Conversely, hyperventilation from fever, anxiety, or high altitude rapidly lowers Pco2, inducing respiratory alkalosis characterized by dizziness, paresthesia, and muscle spasms. These interdependencies highlight Pco2 as a vital bridge between respiratory mechanics and systemic metabolism.
Moreover, changes in Pco2 inform critical decisions in critical care.
A rising Pco2 (hypercapnia) may prompt adjustments in ventilator settings, while a falling Pco2 (hypocapnia) could indicate over-ventilation requiring controlled respiratory support. In metabolic acidosis, cells shift toward bicarbonate regeneration, prompting CO₂ production to buffer pH—visible indirectly through F았바n Curve shifts and Pco2 trends. Physicians use Pco2 alongside pH, HCO₃⁻, and oxygen saturation to diagnose and manage complex disorders with precision.
Factors Influencing Pco2: From Altitude to Disease States Numerous variables shape blood Pco2, demanding nuanced interpretation. At higher altitudes, lower atmospheric oxygen often triggers hyperventilation, reducing Pco2 and sparking acute mountain sickness symptoms. Conversely, in confined spaces with poor ventilation, CO₂ accumulates, elevating Pco2 and inducing cognitive fog or fatigue.
Pathological conditions further modulate Pco2. Chronic respiratory diseases like emphysema shift baseline Pco2 upward due to structural lung damage, whereas asthma attacks may cause erratic surges from airway obstruction. Neurological disorders affecting breathing rhythm—such as stroke or brainstem injury—disrupt chemoreceptor feedback, leading to erratic Pco2 patterns.
Even medications, including opioids and sedatives, depress respiratory drive, directly raising Pco2 and requiring vigilant monitoring.
Understanding these influences ensures accurate diagnosis. A patient with acute asthma exacerbation may present with Pco2 nearing 100 mmHg, indicating severe respiratory failure, while a COPD patient with stable Pco2 isn’t necessarily in distress.
Contextual analysis—age, symptom progression, and supporting lab data—turns Pco2 measurements into actionable clinical insights.
The Clinical Imperative: Why Pco2 Can’t Be Overlooked
Pco2 stands at the intersection of respiratory, metabolic, and neurological function, serving as a real-time barometer of physiological health. From ventilator optimization in intensive care to interpreting routine blood gases in outpatient settings, Pco2’s value is unmatched. Its dynamic nature—responding swiftly to changes in lung mechanics, perfusion, and cellular metabolism—makes it indispensable.Clinicians who master Pco2 interpretation enhance diagnostic accuracy, refine treatment strategies, and ultimately improve patient outcomes. In an era where precision medicine demands nuanced physiological understanding, Pco2 remains a foundational metric—one that quietly governs balance, one breath at a time.



Related Post

Where Is Boston City؟ The Geographic Heart of New England’s Cultural Capital

Trevor Bauer’s Next Move: What’s Next for the Mlb Pitcher Redefining Post-Playcare Craft
Bacteria vs. Eukaryotes: Unlocking the Secrets of Microbial Life
Country Chicken: A Taste of American Tradition in Every Bite

