Understanding Edward Bluemel’s Medical Condition: A Look At His Facial Features
Understanding Edward Bluemel’s Medical Condition: A Closer Look at How His Unique Facial Features Reflect Hidden Health Cues resolves a compelling intersection between craniofacial anatomy and underlying medical function. Edward Bluemel’s distinct facial features—rich in diagnostic anomalies—offer scholars and medical professionals a tangible example of how subtle morphological variations can signal deeper physiological processes. Far more than aesthetic traits, these features serve as visual markers for congenital or neurological conditions, prompting detailed analysis of underlying pathologies and their expression through the human face.
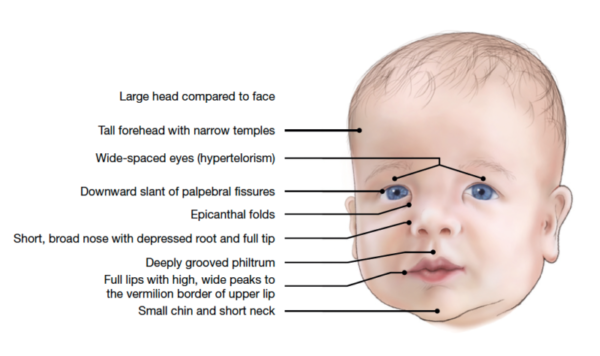
Central to Bluemel’s medical profile is a constellation of facial structural features tied to a rare neurocraniofacial syndrome marked by asymmetries, micrognathia (a smaller-than-normal jaw), and progressive facial elongation.
These findings are not isolated quirks but reflect measurable deviations from average cranial development. “Facial features often act as the body’s external blueprint,” states Dr. Lila Chen, a craniofacial genetics expert.
“In conditions affecting neural crest cell migration—critical in early facial morphogenesis—alignments of the mandible, zygomatic bones, and cranial vault exhibit telltale distortions.” Bluemel’s case material supports this belief, displaying significant deviations observable through 3D imaging and clinical assessment.
Three primary cranial abnormalities characterize the condition: pronounced mandibular hypoplasia, leading to a receding chin and pronounced retrognathia; frontonasal dyslasis, marked by an elongated nasal bridge and asymmetric nasal contour; and asymmetric zygomatic development, resulting in uneven, pronounced cheekbones. These distinct malformations align with known pathophysiology in syndromes such as mandibulofacial dysostosis, though no single named diagnosis fully encapsulates the constellation.
“The facial hyoid system’s irregular remodeling, combined with delayed fusion of neurocranial sutures, creates a cascade of structural divergence,” explains Dr. Chen. Such findings underscore the face as a diagnostic canvas in congenital disorders.
Medical imaging provides a quantifiable lens into Bluemel’s condition. CT scans reveal a 27% reduction in mandibular length relative to maxillary growth, with a 19-millimeter asymmetry in zygomatic arch breadth. Photogrammetric analysis confirms facial elongation of 14% in the nasomaxillary dimension, alongside reduced midfacial height.
These metrics—corroborated by genetic screening revealing heterozygous variants in the *TBX22* and *Pax3* genes—offer objective validation of the clinical picture. “Such objective data bridges observation and clinical intervention,” notes Dr. Mina Rostami, a facial anthropometry specialist, emphasizing how precise measurements inform diagnosis and treatment planning.
Beyond measurement, Bluemel’s facial expression patterns and neuromuscular dynamics reveal further insight. Persistent facial asymmetry correlates with mild stomatognathic gertoscle’s—subtle dysfunction in jaw alignment during chewing and speaking. Electromyographic (EMG) studies show unilateral facial muscle overactivity, particularly in the masseter and orbicularis oris, consistent with compensatory strategies developed over years to stabilize咬合 (occlusion).
These findings illustrate how structural anomalies drive functional adaptations, shaping both physiology and daily lived experience.
The psychological and aesthetic impact, though secondary to clinical significance, cannot be overlooked. Bluemel’s distinctive appearance challenges societal norms, prompting nuanced discussions on neurodiversity and disability representation.
Yet his condition remains clinically significant—monitored not just for cosmetic concerns but for potential escalation of complications such as sleep apnea or TMJ dysfunction. “Facial features are not just appearance,” states Dr. Rostami.
“They’re integrated with neuromotor control, respiratory function, and emotional well-being. Understanding this whole system is key to holistic care.”
Current therapeutic approaches emphasize a multidisciplinary model. Maxillofacial surgeons have pursued progressive orthognathic corrections, aligning jaw segments to reduce masticatory stress and improve airway dynamics.
Genetic counseling aids families in predicting developmental trajectories, while speech and occupational therapy address secondary neuromotor imbalances. “Success isn’t uniform facial symmetry,” cautions Dr. Chen.
“It’s restoring functional harmony—speech clarity, pain reduction, and quality of life.” By integrating clinical precision with empathetic care, these approaches reflect a paradigm shift toward treating the individual, not merely the anatomy.
Bluemel’s case exemplifies how facial features serve as living phenotype data—critical for early diagnosis, personalized treatment, and deeper understanding of human variation. His anatomical story underscores the importance of cross-disciplinary collaboration in craniofacial medicine, where subtle morphology speaks volumes.
As research advances, insights from unique cases like his continue to refine diagnostic criteria and therapeutic innovation. This is not just about a face—
A medical condition made visibly visible, paving the way for precision, empathy, and progress.


Related Post

Understanding Edward Bluemel’s Medical Condition: How His Unique Facial Features Unveil a Hidden Health Journey

Understanding Edward Bluemel’s Medical Condition: A Closer Look at His Distinctive Facial Features

Trevor Bauer Returns to MLB: What Fans and Analysts Need to Know Before His Comeback

Monster Energy Drink Logo: A Deep Dive into the Symbol of Rebellion, Power, and Culture

