Understanding Acute Lymphoblastic Leukemia (ALL) In Children
Understanding Acute Lymphoblastic Leukemia (ALL) in Children: The Most Common Childhood Cancer}}
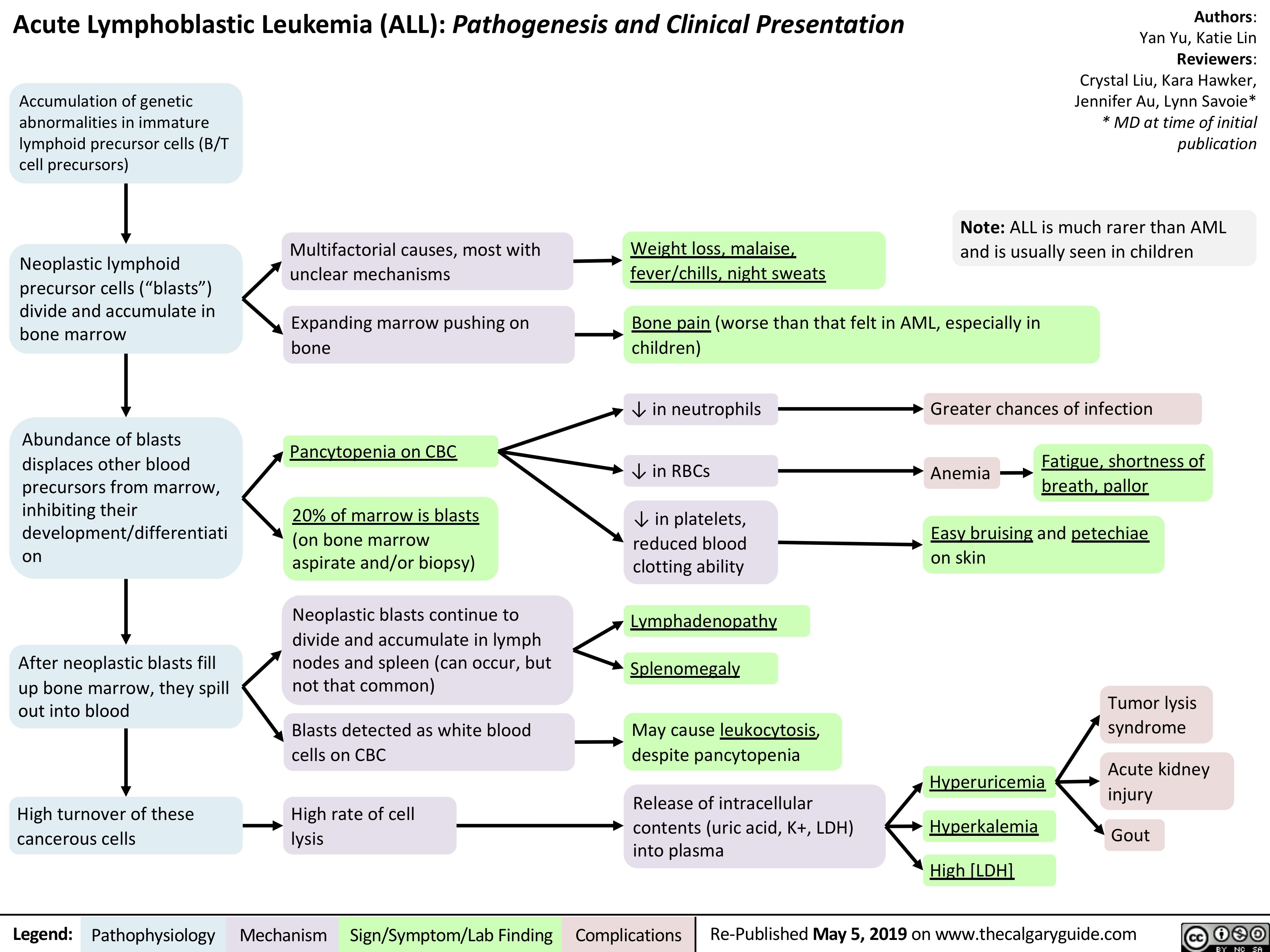
Acute Lymphoblastic Leukemia (ALL) stands as the most prevalent childhood cancer, affecting approximately 1 in 25,000 children under the age of 15. This aggressive form of blood cancer arises when immature lymphocytes—blood cells destined to mature into B cells or T cells—begins to multiply uncontrollably in the bone marrow, crowding out healthy blood cells and disrupting normal body function. Unlike many adult cancers, ALL primarily strikes children and adolescents, with peak incidence occurring between 2 and 5 years of age.
Despite its severity, rapid advances in diagnosis and treatment have transformed ALL from a frequently fatal diagnosis into one with a strong potential for long-term remission, especially when detected early.
The Biology and Classification of Pediatric ALL
ALL is classified based on the type of lymphoblast involved—either lymphoblasts of B-cell or T-cell origin—accounting for roughly 85% of cases being B-cell derived and 15% T-cell. Within these categories, additional subtypes and genetic markers further refine prognosis and treatment. Common genetic abnormalities include the Philadelphia chromosome (BCR-ABL1 fusion), hyperdiploidy, and specific mutations in genes like NMG6 or KMT2A.“These molecular fingerprints not only guide therapy but also reveal the underlying complexity of a disease once viewed solely as a “white blood cell cancer.”
Clinical presentation varies but often includes symptoms stemming from bone marrow crowding: persistent fatigue, pale skin, easy bruising, fever, infections, frequent nosebleeds, and bone or joint pain—signs of marrow failure and leukemic cell infiltration. On physical exam, hepatosplenomegaly and lymphadenopathy may be observed, prompting deeper investigation. Early recognition, supported by routine pediatric screening and awareness, remains pivotal for favorable outcomes.
Diagnosis: From Blood Tests to Genetic Profiling
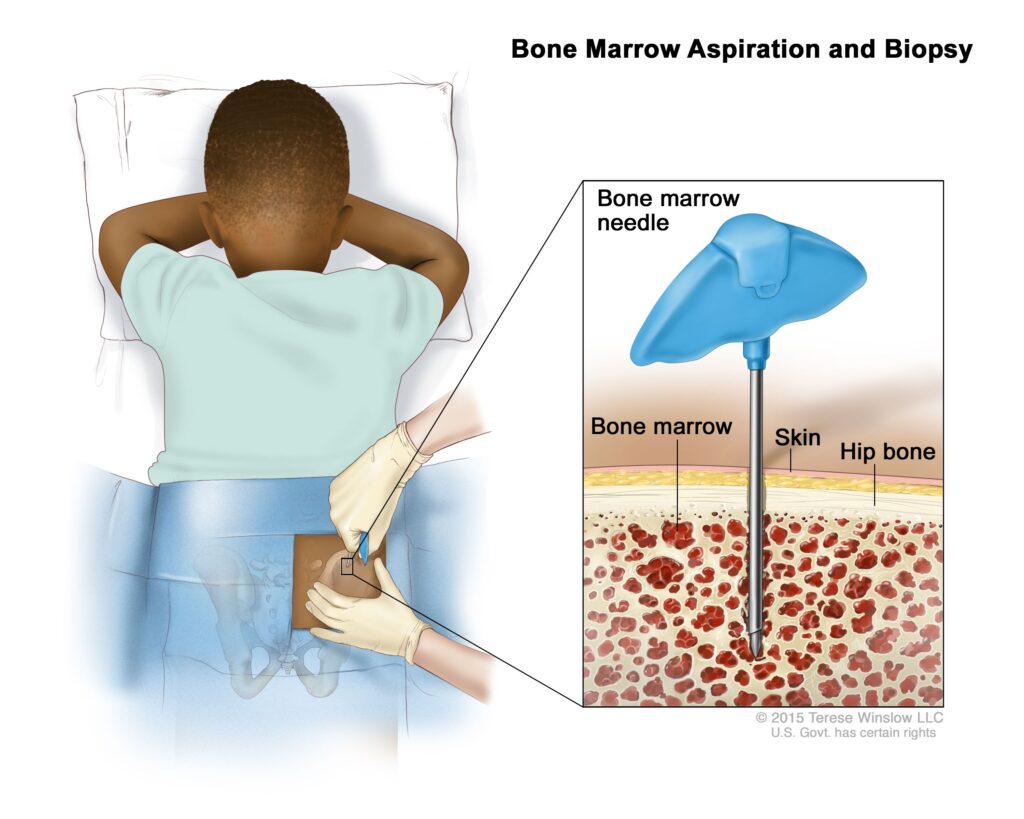
Accurate diagnosis begins with a complete blood count revealing elevated white blood cell counts often immature and lacking developed lymphocytes.A confirming bone marrow biopsy—retrieving cells from the hip bone—provides the definitive evidence through perphery examination and cytogenetic analysis. Stadial classification, using the International Pediatric ALL Classification system, integrates key markers: leukocyte count, presence of leukemic blasts, central nervous system involvement, and specific genetic abnormalities. “Modern diagnostic tools now allow us to parse the DNA of浸润 leukemic blasts with unprecedented precision,” notes Dr.
Elena Torres, a pediatric oncologist at Boston Children’s Hospital, “turning once-unknown subtypes into actionable targets.”
Advances in molecular testing have revolutionized diagnostic accuracy. Fluorescence in situ hybridization (FISH) and next-generation sequencing identify high-risk genetic changes long before symptoms worsen, enabling risk-adapted treatment strategies. For example, the presence of the MLL gene fusion significantly increases relapse risk, prompting intensified therapy.
These insights underscore the shift from a one-size-fits-all approach to personalized medicine in pediatric ALL management.
Treatment Breakthroughs Driving Remission Rates Above 90%
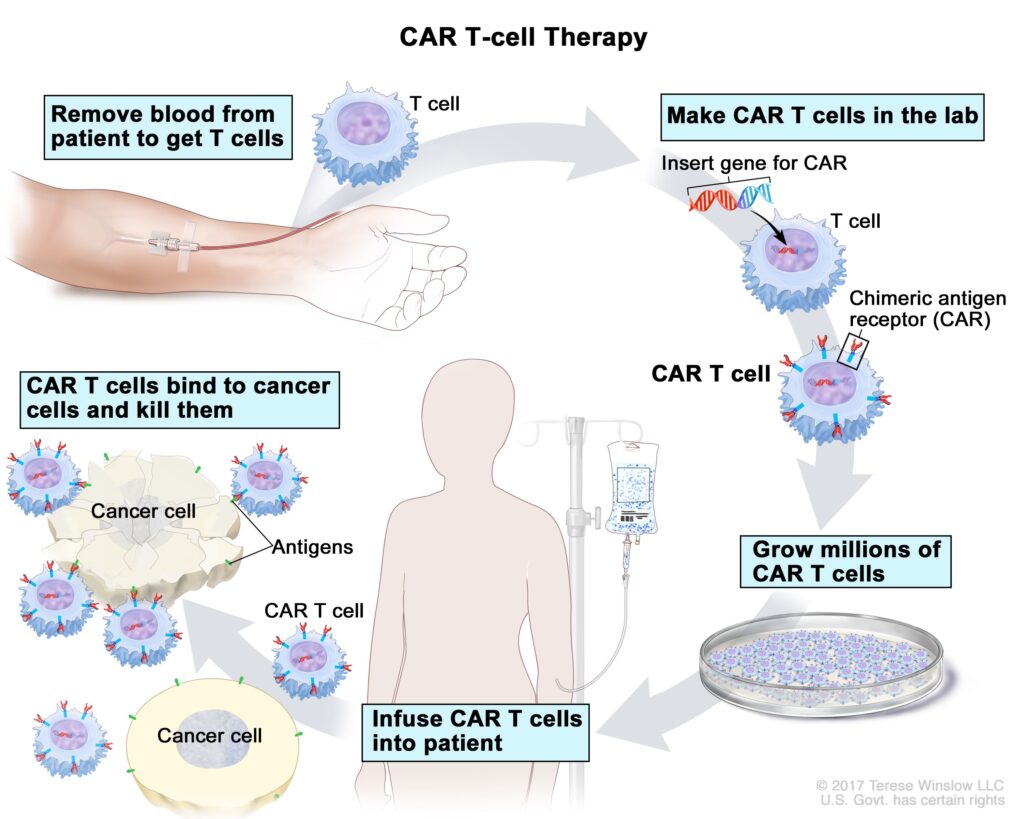
The foundation of modern ALL treatment rests on multi-phase chemotherapy regimens, often termed “induction,” “consolidation,” and maintenance phases. Induction therapy rapidly reduces leukemic blasts, achieving remission in >90% of cases, followed by consolidation therapy to eliminate residual disease, and prolonged maintenance to prevent relapse. Corticosteroids, anthracyclines, and dexamethasone remain cornerstone drugs, paired with targeted agents like blinatumomab—a monoclonal antibody that redirects immune cells to destroy leukemic blasts—and tyrosine kinase inhibitors for Philadelphia chromosome-positive cases.Emerging therapies, including chimeric antigen receptor (CAR) T-cell therapy, are redefining expectations, especially for relapsed or refractory disease. “CAR T has changed the landscape—sometimes we’re not just curing, but offering hope where once there was only facing a lifelong battle,” says Dr. Raj Patel, head of the ALL program at St.
Jude Children’s Research Hospital.
Clinical trials continue to refine protocols, balancing aggressive eradication with minimizing long-term toxicity. Late effects such as cardiac dysfunction, growth delays, and secondary malignancies are vigilantly monitored.
The goal is not only remission but also a high-quality life beyond treatment—emphasizing survivorship care with dedicated pediatric oncology subspecialists.
Living with ALL: Family Impact and Multidisciplinary Support
The diagnosis of ALL reverberates far beyond the clinic. For families, the journey encompasses intensive hospital stays, complex medication schedules, emotional strain, and financial burden. Support networks—ranging from community organizations to hospital-based social workers—play a vital role in easing the transition.Many centers now offer integrated psychosocial services, school reintegration programs, and caregiver education. “Hearing a child’s voice during treatment—sometimes through a phone screen, sometimes just in spirit—reminds us that healing is emotional as much as physical,” reflects Nancy Kim, a childhood leukemia grateful survivor and advocate. The creation of centralized pediatric cancer centers, combining clinical excellence with compassionate care, has proven essential in addressing the holistic needs of children and their families.
Prevention remains limited, but early symptom awareness empowers timely medical attention. Routine pediatric visits ensure nothing goes unnoticed. While the exact cause of most ALL is unknown, genetic predisposition and environmental exposures may play roles—remaining active areas of research.
Acute Lymphoblastic Leukemia in children is a complex, high-stakes disease, but one marked by extraordinary progress. From profound biological insights to transformative therapies, medicine continues to rewrite survival odds. With unwavering research, compassionate care, and global collaboration, the future for children with ALL grows increasingly bright—where cancer is no longer a sentence, but a challenge met with resilience and hope.

Related Post

Upgrade Your IPhone: Trade In the iPhone 11 for the 13 Pro and Unleash Next-Level Performance and Design

Barry Weiss Wife: The Untold Story Behind The A&E Star’s Personal Life

Credit Agricole Singapore: The Unseen Engine Driving Southeast Asia’s Financial Future

At 6'3": The Unbelievable Stature That Defined Mike Tyson’s Dominance

