Prednisone for Cough: When Steroids Fight Airway Inflammation — Uses, Risks, and What Patients Should Know
Prednisone for Cough: When Steroids Fight Airway Inflammation — Uses, Risks, and What Patients Should Know
Reductions in breathing comfort can strike suddenly and disrupt even the simplest daily routines. For persistent, inflammatory coughs that resist typical treatments, prescribers may consider an unexpected ally: prednisone. As a potent corticosteroid, prednisone targets airway inflammation at its root, offering relief when cough stems from conditions like asthma, chronic throat irritation, or post-infectious hyperreactivity.
Yet, its use demands careful consideration—balancing therapeutic benefits against significant risks. This article unpacks the current understanding of prednisone in managing cough, outlining its approved uses, dangers, and essential patient guidance.
How Prednisone Works to Treat Cough: Targeting Inflammation at Its Source
Prednisone is a synthetic glucocorticoid designed to mimic the body’s natural anti-inflammatory hormones.By suppressing immune and inflammatory responses, it reduces swelling, mucus production, and irritation in the respiratory tract—key drivers of both acute and chronic cough. When inflammation triggers nerve sensitivity or narrows airways, prednisone’s action helps restore normal breathing and diminish the persistent urge to cough. Respiratory specialists emphasize this mechanism is most effective in cough linked to measurable inflammation.
“Prednisone doesn’t treat a cough directly; it dampens the underlying process that generates it,” explains Dr. Elena Marquez, a pulmonary medicine expert. “This makes it especially useful in conditions like laryngopharyngeal reflux, steroid-responsive cough variants, or infections followed by anti-inflammatory remodeling.” Prednisone is typically reserved for cases where coughing persists despite first-line therapies—such as inhaled bronchodilators or short-course antibiotics—because uncontrolled inflammation can signal deeper pathology requiring targeted immune modulation.
When Is Prednisone Prescribed for Cough? Key Indications
Prednisone for cough is not a default option but a strategic tool in specific clinical scenarios. The most common indications include: - **Steroid-responsive non-productive cough**: A subset of patients experience dramatic improvement with low-dose corticosteroids.Studies report symptom relief in 40–70% of these cases, particularly when cough follows viral infections or refracts from standard therapy. - **Inflammatory airway diseases**: Conditions like eosinophilic bronchitis or asthma-related cough benefit from prednisone’s ability to reduce airway hyperresponsiveness. - **Post-viral cough syndromes**: Some patients develop persistent cough after respiratory infections; prednisone may accelerate resolution when inflammation remains clinically evident.
- **Foreign body aspiration or granulomatous inflammation**: In rare instances, it helps calm the immune reaction and reduce airway obstruction. Importantly, prednisone is never used for cough without an inflammatory basis. Misuse—such as treating benign or infectious coughs without confirmed inflammation—poses unnecessary risk and invites resistance.
Dosage, Duration, and Administration: Getting It Right
Setting the right dose and schedule is critical to efficacy and safety. Prednisone’s pharmacokinetics allow flexibility—oral tablets or cautious intravenously—but guidelines emphasize starting low and tapering gradually. - **Initial dose**: For most patients, a 30–40 mg dose once daily is standard for inflammation-driven cough.- **Response monitoring**: Improvement often begins within 24–72 hours, but public awareness lags—patients should track cough frequency, severity, and any side effects like jitteriness or disrupted sleep. - **Tapering protocol**: Dipping into too-high doses too quickly heightens adverse effects. A gradual taper over 1–4 weeks aligns with the body’s adjustment, reducing withdrawal-related rebound inflammation or adrenal suppression.
- **Avoid abrupt discontinuation**: Stopping prednisone suddenly—even after only a few days—can trigger adrenal crisis, especially in long-term users. Healthcare providers stress that prednisone is not a “quick fix.” Its success depends on proper dosing, duration, and ongoing symptom monitoring, often in tandem with other therapies like antihistamines or mucolytics.
Serious Risks and Side Effects: Weighing Benefits Against Dangers
While effective, prednisone carries a spectrum of acute and chronic risks that must not be overlooked.Clinicians weigh these carefully, especially in vulnerable populations. - **Metabolic disturbances**: Elevated blood glucose, fluid retention, and weight gain may occur even with short courses, particularly in diabetics or those predisposed to metabolic syndrome. - **Osteoporosis and bone weakening**: Prolonged use increases fracture risk, though even short durations require monitoring, especially in postmenopausal women.
- **Immunosuppression**: Suppressed immune function raises infection susceptibility—ranging from minor skin eruptions to life-threatening respiratory illnesses. - **Psychiatric effects**: Mood swings, anxiety, or insomnia can emerge, particularly at higher doses. - **Cardiovascular strain**: Include spikes in blood pressure and fluid overload, demanding vigilance in patients with heart disease.
“Prednisone is a powerful tool, but it’s not benign,” cautions Dr. James Holloway, a rheumatology specialist. “Patients need clear understanding of both short-term symptom relief and potential long-term impacts—especially if used beyond 2–3 weeks without close oversight.” These risks are dose- and duration-dependent.
Low, short-term regimens carry lower danger, but cumulative exposure significantly amplifies concerns—particularly for older adults or those with comorbidities.
Who Should Avoid Prednisone for Cough? Key Contraindications and Cautions
Prednisone is contraindicated or highly discouraged in specific populations and conditions: - **Active infections**: Including tuberculosis, HIV with uncontrolled replication, or unmanaged HIV pneumonia—steroids can mask symptoms and weaken immune defense.- **Untreated hypertension or cardiovascular disease**: Prednisone’s fluid-retaining and pressure-elevating effects can worsen outcomes. - **Diabetes mellitus**: The drug raises blood sugar; even brief courses require glucose monitoring. - **Pregnancy and lactation**: While sometimes medically needed under strict guidance, risks to fetal development and breast milk contamination necessitate caution.
- **Gastrointestinal ulcers**: GCS steroids increase bleeding risk and may exacerbate existing lesions. Patients on concurrent steroid therapies—such as corticosteroid inhalers with systemic use—require careful coordination to avoid additive immunosuppression or Cushingoid symptoms.
Practical Tips for Patients: Using Prednisone Safely and Effectively
To maximize benefit and minimize harm, patients should adopt proactive strategies when prescribed prednisone: - **Never self-adjust**: Doses must follow the prescriber’s plan—even a single missed day or wrong-handed adjustment risks instability.- **Track symptoms closely**: Use a daily log recording cough patterns, energy levels, mood, and side effects to share with providers. - **Communicate openly**: Report signs of infection, unusual fatigue, or mood changes promptly. - **Strengthen defenses**: Eat a balanced diet rich in calcium and vitamin D, stay hydrated, and limit salt intake during treatment.
- **Prioritize tapering**: Resist the urge to stop abruptly, even if symptoms ease—work with your doctor to plan a gradual reduction. Healthcare systems increasingly integrate patient education tools—digital trackers, short videos, and optimized prescription counseling—to bridge the gap between clinical guidance and real-world use.
Prednisone for Cough: A Tool of Precision, Not Panacea
Prednisone remains a vital intervention for cough rooted in inflammation—offering relief when other avenues fail.Yet its power demands respect: high efficacy paired with significant risks requires vigilant monitoring and individualized care. Patients and providers alike must balance rapid symptom control with long-term safety, guided by evidence, oversight, and clear communication. When used thoughtfully, prednisone transforms a disruptive, often invisible struggle into a manageable condition—restoring breathing, dignity, and normalcy, one balanced dose at a time.



Related Post

Cyclone Hollanda: Tracking the Storm, Assessing the Damage, and What Matters in the Aftermath
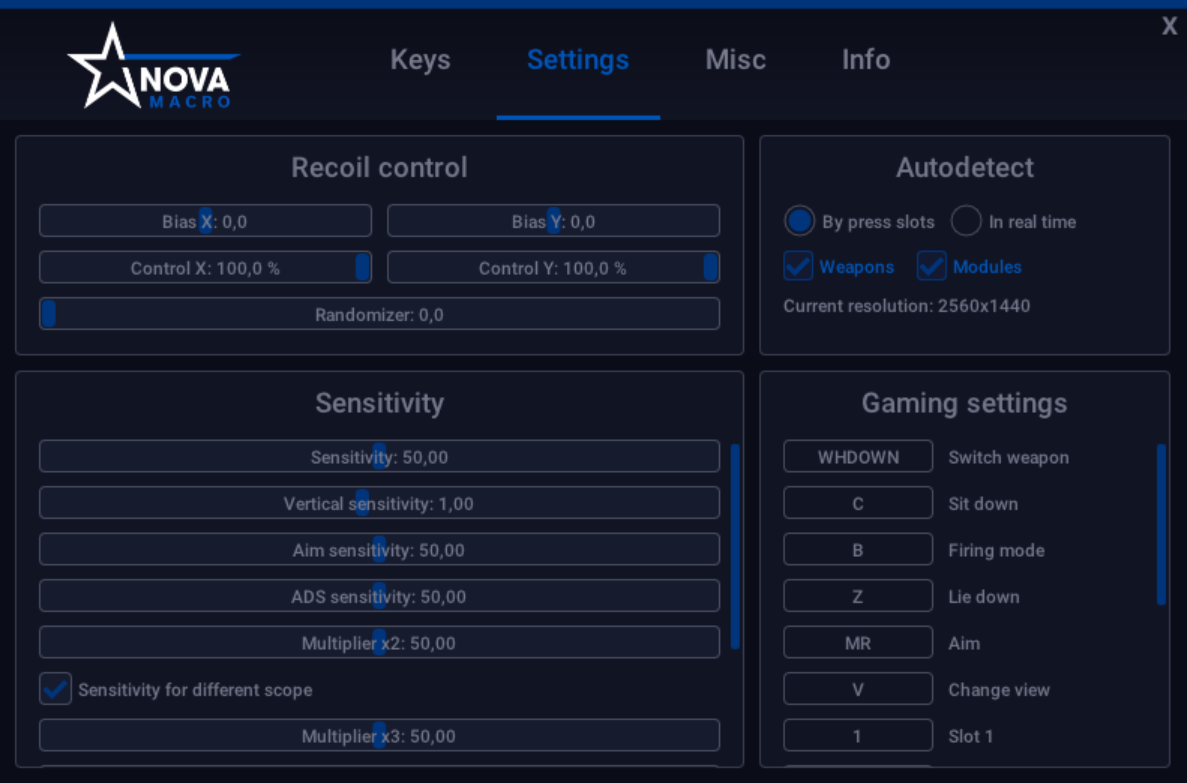
PUBG Mobile No Recoil Hacks: Exposing the Hidden Dangers Behind No Recoil Tricks

Unveiling Creepshot Forums: The Hidden Dangers of Creepshot Culture and How to Stay Safe

🔥 Viral MMS HD Videos: Deciphering the Phenomenon Driving Millions—Trends, Risks, and Digital Insights

