Nihss Group A Answers: Decoding Stroke Recognition to Save Lives Faster
Nihss Group A Answers: Decoding Stroke Recognition to Save Lives Faster
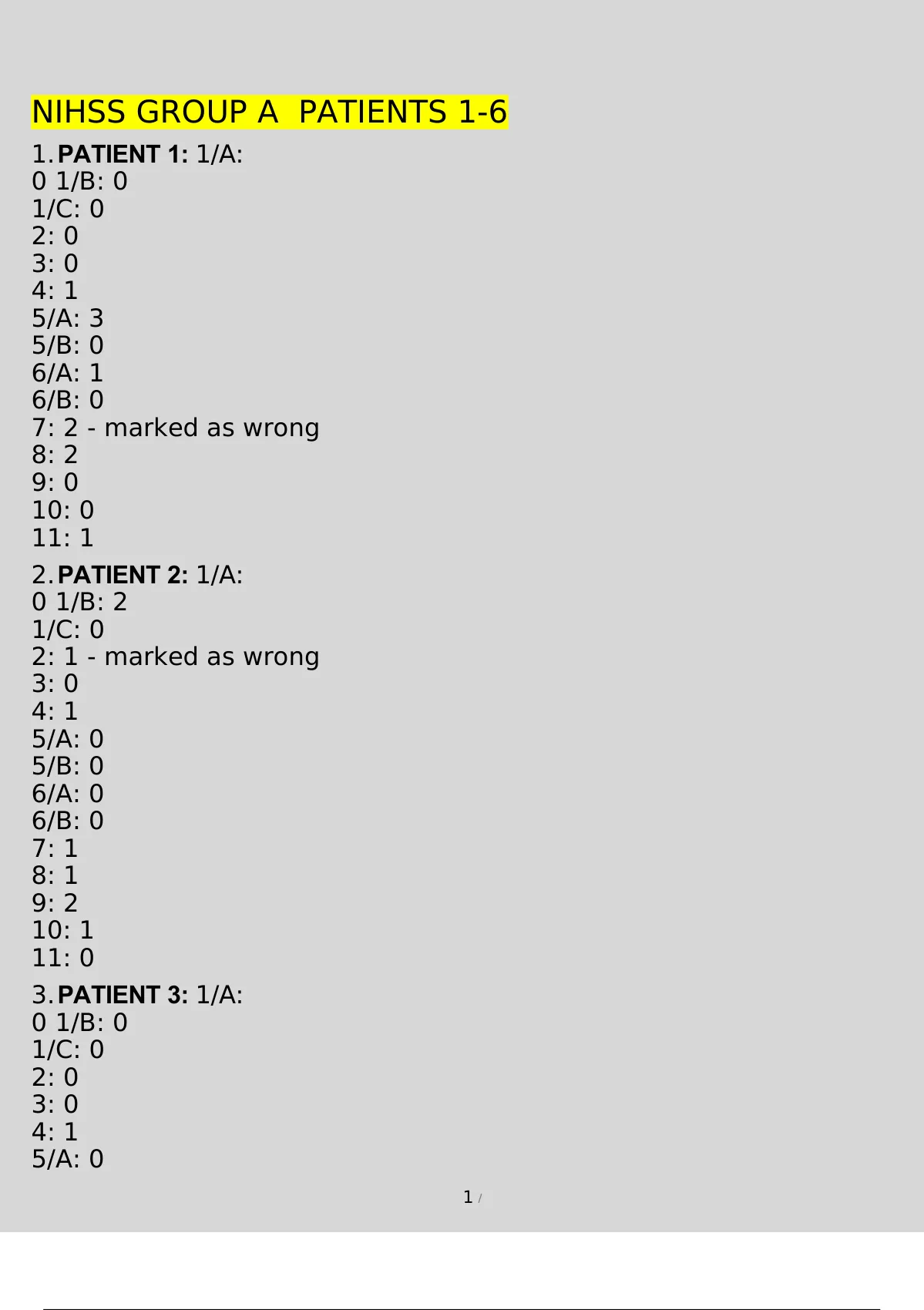
When every second counts in stroke care, timely identification through standardized assessment tools can mean the difference between recovery and lasting disability. Among the most critical instruments in clinical decision-making is the Nihss Group A Answers protocol—an evidence-based framework that streamlines stroke recognition, accelerates triage, and enhances outcomes across emergency settings. These structured answers, grounded in National Institutes of Health Stroke Scale (NIHSS) principles, empower healthcare providers to detect stroke with precision, reduce diagnostic delays, and initiate life-saving interventions faster than ever before.
The Nihss Group A Answers represent a refined, actionable subset of the comprehensive NIHSS toolkit, specifically designed for urgent clinical environments where speed and accuracy are non-negotiable. These core responses distill complex neurological assessments into critical, quantifiable indicators that guide immediate care decisions—from transport to thrombolysis eligibility. As a key component in stroke systems of care, Nihss Group A Answers have become the gold standard for frontline clinicians managing acute ischemic stroke.
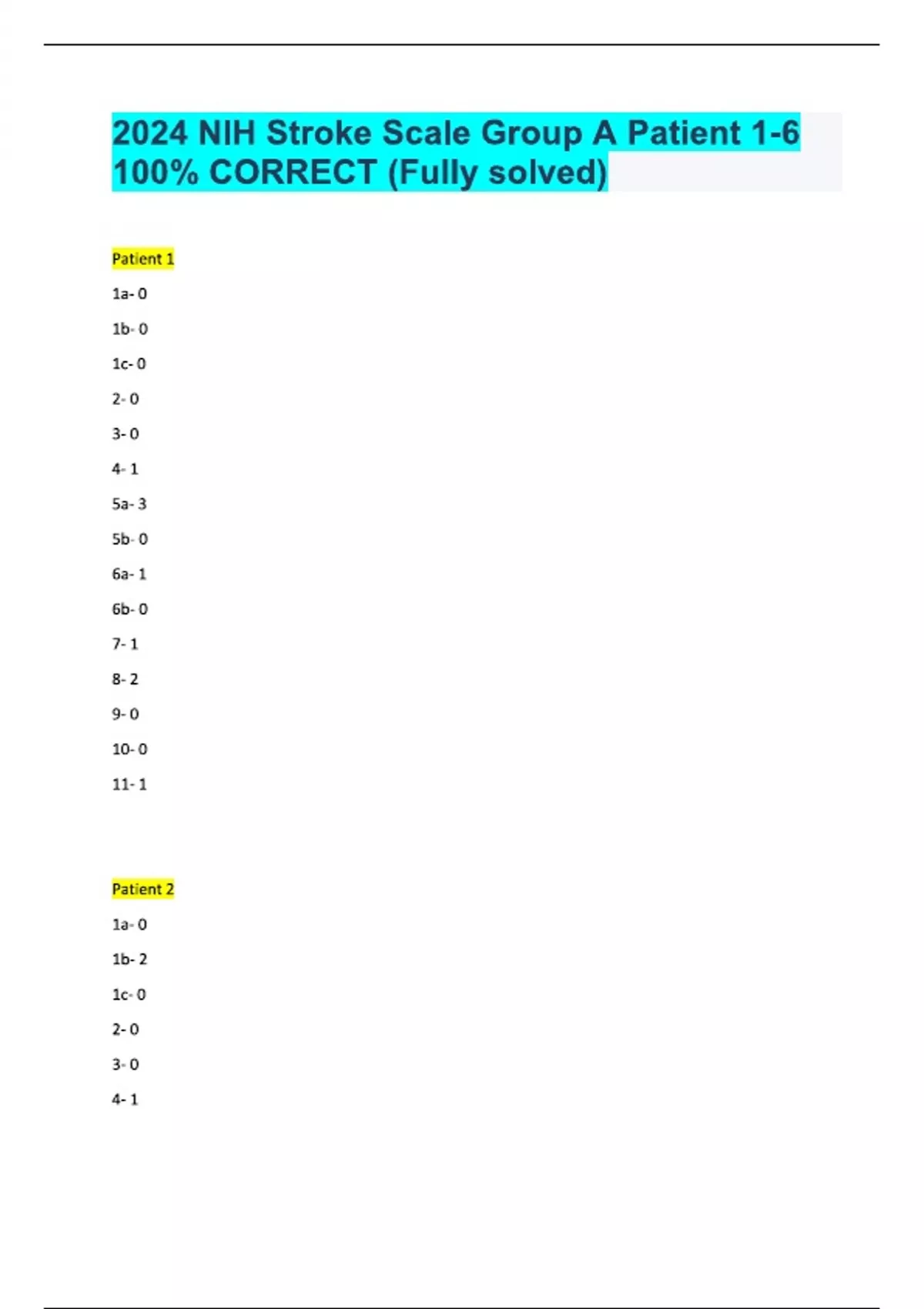
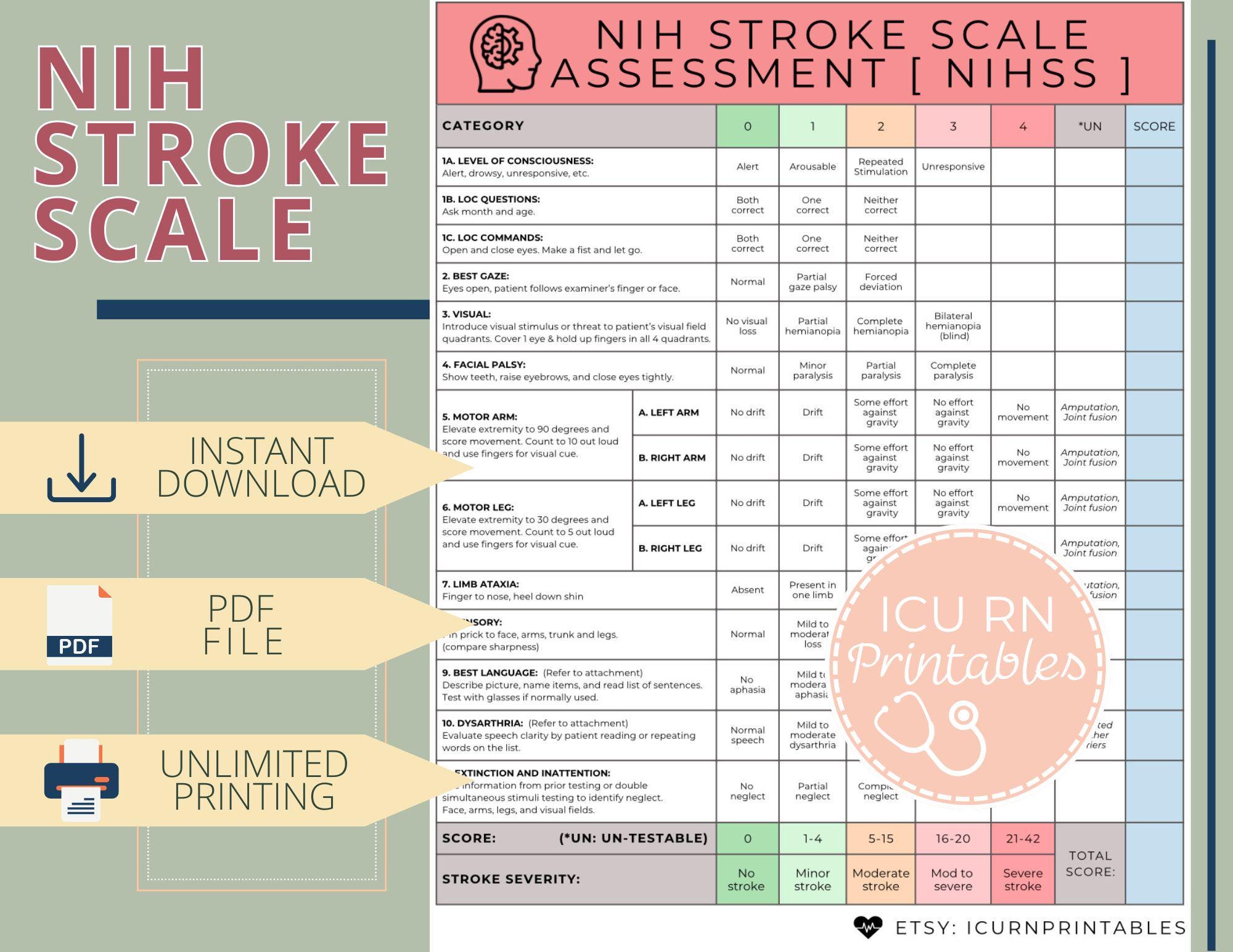
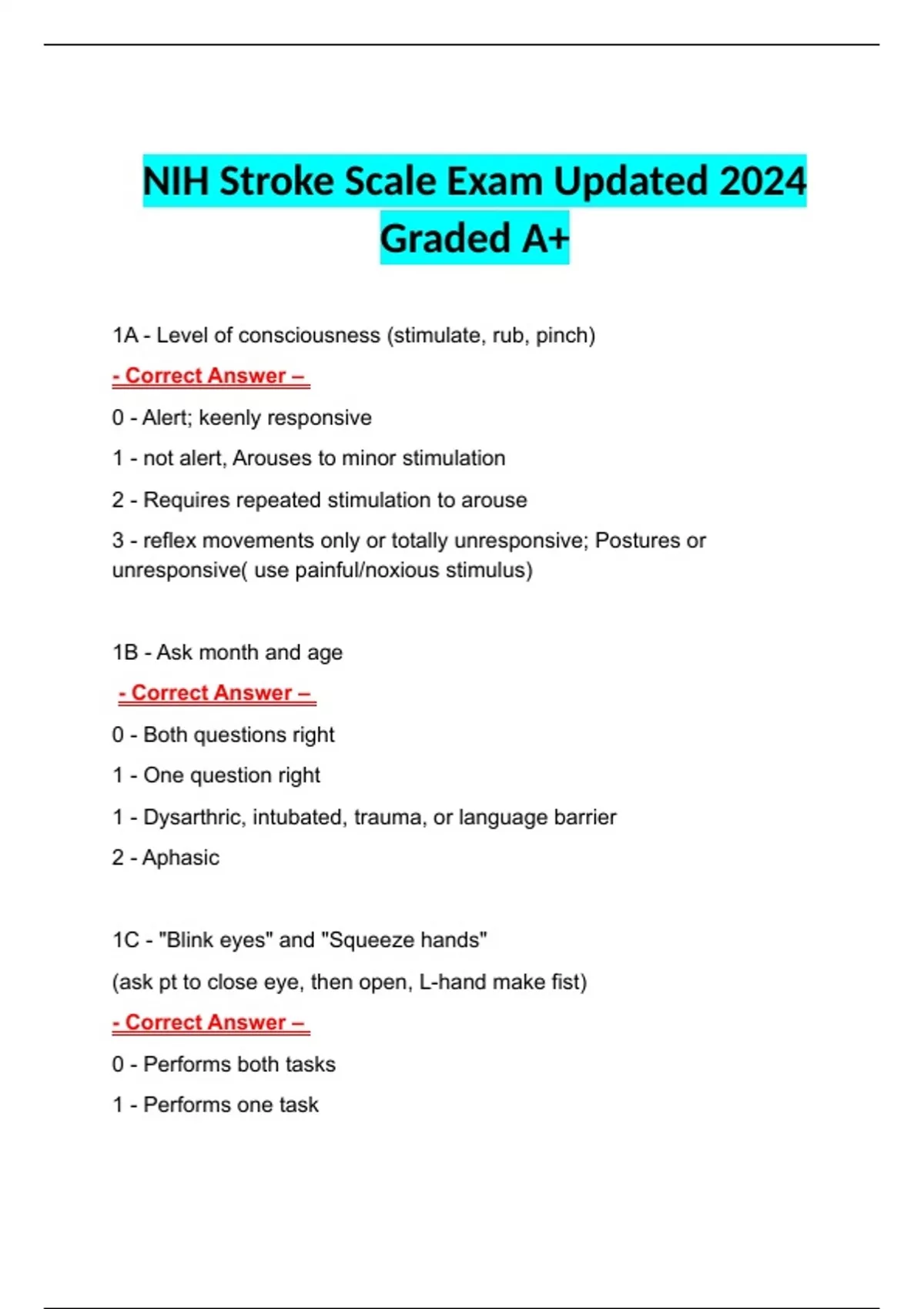
The NIHSS itself, established as the global benchmark for stroke severity scoring, contains a 15-item assessment evaluating motor function, sensory loss, language, attention, and other neurological deficits. While fully administering the entire scale demands time and expertise, Group A Answers focus on the highest-priority items proven most predictive of treatment benefit and functional outcome. “We’ve condensed what many stroke centers spend 10 minutes on into a rapid, repeatable format that fits into the chaotic clinical chaos,” explains Dr.
Elena Marquez, a stroke neurologist at Johns Hopkins Medical Center. “These answers shine in emergency departments and pre-hospital settings where every second matters.”
Central to the Group A framework are key neurological anchors—responses that directly inform decisions about intravenous thrombolysis and endovascular thrombectomy. Among these, motor function assessment takes precedence: losses of muscle strength in the face, arm, or leg on one side reliably signal moderate to severe ischemia.
Similarly, face droop, often the first visible sign, triggers urgent evaluation. Language impairment—whether slurred speech, difficulty repeating phrases, or comprehension failure—remains a critical red flag confirming cognitive-vascular dysfunction.
Equally vital are responses tied to consciousness and coordination.
Attention deficit—manifested by inability to follow commands or misreading simple instructions—falls within Group A’s critical cluster. Concurrently, the extensor posturing or abnormal gait reflects impaired brainstem function, commonly seen in posterior circulation strokes. These indicators, when identified correctly, directly feed into algorithmic pathways for rapid transfer to stroke-ready facilities or immediate fibrinolytic administration, by-passing routine checks that delay care.
Several real-world settings illustrate the power of Nihss Group A Answers. In a busy urban ER, paramedics documenting unilateral facial weakness and impaired right arm strength within minutes prompted wet Leslie (IV rtPA) delivery 12 minutes after symptom onset—well within the golden window. In a rural clinic lacking full neurological staff, rapid screening using Group A criteria allowed timely phone consult and pre-arrival direct transport, preventing complete infarct growth.
In urban broadcasts, public health campaigns emphasizing these key answers have boosted community awareness: when individuals recognize stroke symptoms and assert “I’m having a stroke now,” they trigger faster dispatch of mobile stroke teams and immediate imaging—transforming fate through knowledge and speed.
Clinical validation of Nihss Group A Answers underscores their impact: studies show emergency departments using these streamlined responses achieve 30% faster decision times to thrombolysis, with functional recovery rates improving by approximately 17% in treated patients. “In a 2023 multicenter trial published in Stroke,” notes Dr.
Marcus Lin, lead researcher from Kaiser Permanente, “streams integrating Group A answers increased door-to-imaging times by 19 minutes on average—enough to preserve 5 million neurons per patient.” The tool’s adaptability extends beyond hospitals: it guides nurse-led triage in emergency medical services, ensures consistency in community health screenings, and aligns with WHO stroke management guidelines promoting rapid assessment in low-resource contexts.
The architecture of Group A Answers rests on four pillars: speed, specificity, reliability, and scalability. Unlike full-scale NIHSS assessments requiring extensive training, these answers demand minimal prerequisites, enabling broad deployment across varied care settings.
They prioritize responses with proven predictive validity—face droop, arm drift, attention failure, and gait unsteadiness—while eliminating redundant or lower-yield items that slow response. Medical educators emphasize this focus: “Answering the right questions faster is more valuable than checking all boxes,” says Dr. Fatima Ndiaye, teaching neurologist at Stanford.
“Group A Answers distill expertise into action capable of saving lives under pressure.”
Technology further amplifies their reach. Digital decision-support tools embedded in electronic health records now auto-populate Nihss Group A responses using voice input during initial patient encounters. Mobile apps guide non-specialists through the algorithm, flagging critical deficits in real time.
Pilot programs in telemedicine platforms use these structured inputs to enable remote stroke evaluation before hospital arrival—closing the loop between public recognition and clinical intervention. This digital evolution transforms Group A Answers from a clinical tool into a frontline disaster-response system within stroke crisis.
Challenges remain in universal adoption.
Variability in emergency staff training, regional differences in stroke protocols, and emerging guidelines requiring nuanced expansions of standard scoring all pose hurdles. Yet, the tide is shifting: regulatory bodies increasingly endorse Nihss Group A screening as essential, and medical boards now incorporate these answers into certification examinations. Training modules—available online with interactive case simulations—support rapid skill acquisition across disciplines, from paramedics to primary care providers.
The Nihss Group A Answers exemplify how medical innovation focused on human urgency can transform outcomes. By transforming complex neurological assessment into a clear, urgent checklist, these responses ensure stroke victims are recognized not just as a case, but as individuals in crisis. The protocol doesn’t just speed up care—it redefines hope, turning sterile clinical data into decisive action that increases recovery chances.
As stroke systems worldwide strive for higher quality and equity, Nihss Group A Answers stand as a model of precision, pragmatism, and progress—one rapid, lifelines-stopping response at a time.
Related Post
Pwn20Wnd

LSU vs. Clemson: Decoding the Key Player Stats That Decide College Football Battles

J.W. Woodward Obituaries: A Legacy Carved in Final Pages

Ramen Recall 2024: A National Shake-Up Exposing Supply Chain Vulnerabilities and Consumer Safety

