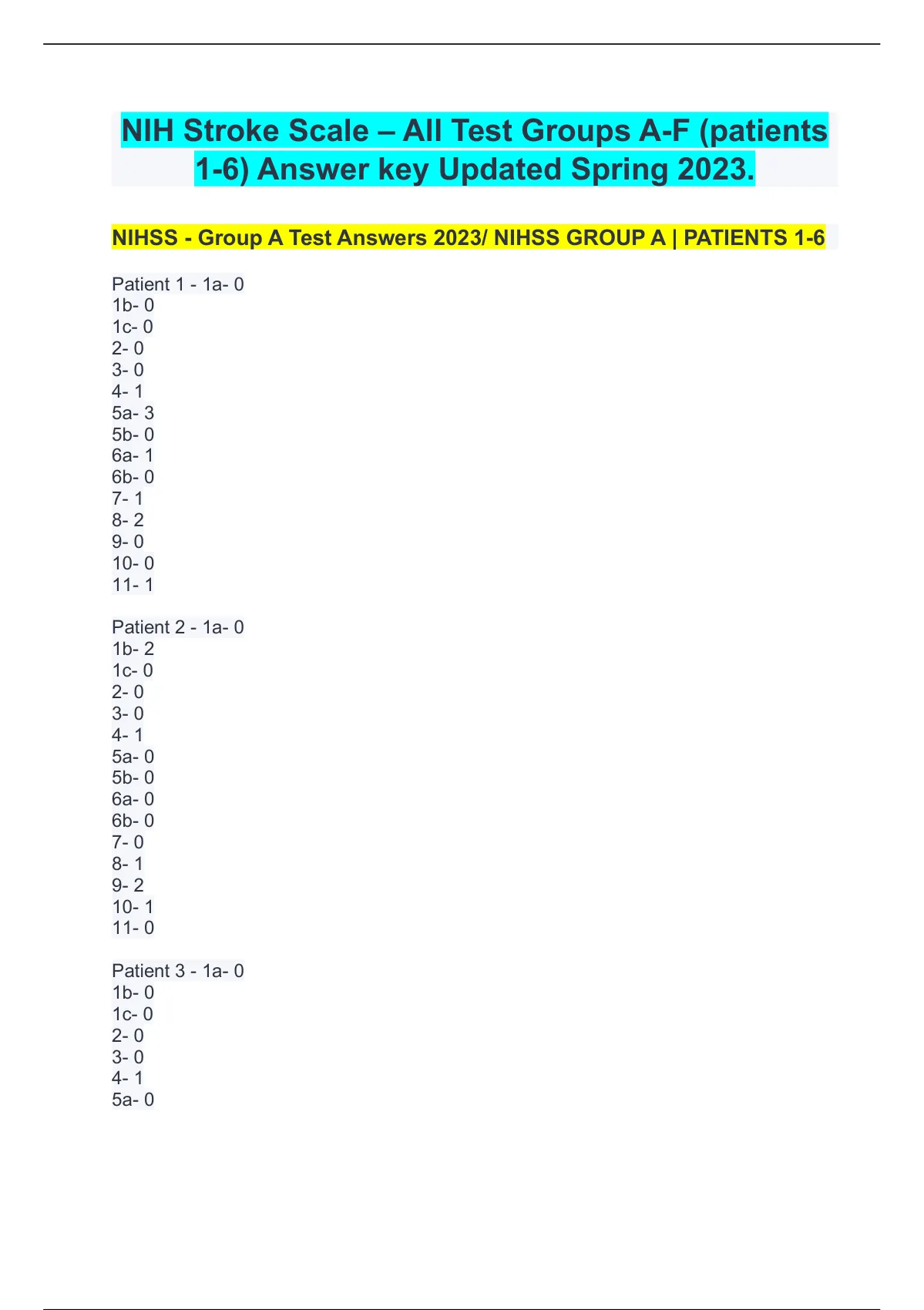
Arrhythmia vs. Dysrhythmia: The Critical Line Between Healthy and Wildly Unstable Heartbeats
Arrhythmia vs. Dysrhythmia: The Critical Line Between Healthy and Wildly Unstable Heartbeats
In the intricate ballet of cardiac function, the distinction between arrhythmia and dysrhythmia lies at the heart of cardiovascular health—yet remains shockingly misunderstood. Though often used interchangeably, these terms represent scientifically distinct classifications with profound implications for diagnosis, treatment, and patient outcomes. Architecting a clearer understanding reveals not just a difference in language, but a vital divergence in clinical significance.
Arrhythmia signals a deviation from normal sinus rhythm, while dysrhythmia encompasses broader, often reversible irregularities that may foreshadow serious cardiac dysfunction. Grasping this nuance is essential—both for medical professionals and patients seeking clarity in navigating heart rhythm disorders. Understanding Rhythmic Footprints: The Core Difference At its foundation, arrhythmia denotes any abnormal heart rhythm, whether too fast (tachyarrhythmia), too slow (bradyarrhythmia), or irregular in timing and force.
These deviations disrupt the sinoatrial node’s pacing, producing beats that deviate from the expected 60–100 beats per minute under rest. In contrast, dysrhythmia traditionally refers to unstable, irregular rhythms not fully classified as a primary arrhythmia but indicating electrical instability—often transient and typically linked to underlying stress, drugs, or metabolic imbalances. <
This distinction guides critical diagnostic pathways, ensuring clinicians do not overlook reversible causes behind what might initially appear as a chronic arrhythmia. Classification Systems: Mapping the Arrhythmia-Dysrhythmia Spectrum 医学界 recognizes arrhythmia and dysrhythmia through structured classification systems that enhance clinical precision. The most widely referenced is the Sinclair Classification, which divides cardiac rhythm disturbances into definitive arrhythmias and dysrhythmias based on electrophysiological origin and clinical relevance.
Within arrhythmia, categories span: - Atrial fibrillation (AF)—the most common persistent arrhythmia, marked by disorganized atrial electrical activity and chaotic conduction - Ventricular tachycardia (VT)—a life-threatening rhythm originating below the atrioventricular junction - Bradycardia with sinus node dysfunction or atrioventricular block - Premature beats—extra impulses often labeled premature ventricular contractions (PVCs) or prematureAtrial contractions (PACs) Conversely, dysrhythmia clusters involve: - Sinus node dysfunction (sick sinus syndrome), leading to inappropriate bradycardia - Levt right bundle branch block (LRBB) or other conduction delays - Various forms of atrial or ventricular ectopy without sustained instability - Metabolic-related irregular beats triggered by hypoxia, acidosis, or electrolyte shifts <
Arrhythmias typically stem from intrinsic cardiac substrate changes: fibrosis from prior myocardial infarction, ion channel pathology altering depolarization, or autonomic modulation throwing the autonomic nervous system out of balance. In contrast, dysrhythmias often arise from extrinsic, environmental, or metabolic forces—acute blood loss lowering blood pressure, alcohol-induced electrolyte shifts, or drug-induced ST-segment changes. <
For instance, a patient with persistent AF faces long-term anticoagulation and rate/rhythm control, whereas someone with transient ectopy due to dehydration may benefit from rehydration and observation. Clinical Presentation: From Silent to Survival-Threatening Signs Patients with arrhythmias often present with palpitations, dizziness, or exercise intolerance—symptoms tied directly to rhythm disruption. In advanced cases, sustained arrhythmias strain the heart, reducing output and precipitating heart failure.
Dysrhythmias, however, frequently manifest subtly—lightheadedness after rising, fatigue, or near-syncope—because their instability is episodic and self-limiting. A well-documented case reported in the *Journal of Cardiac Electrophysiology* illustrated a 58-year-old woman whose fainting episodes arose not from chronic ventricular arrhythmia, but from transient sinus pause and corrected electrolyte imbalances, resolved only after hydration and targeted electrolyte replacement. < Ignoring their quiet pain can cost lives.>> Diagnostic Tools: Precision in Detecting Arrhythmia vs. Identifying Dysrhythmia Electrocardiography (ECG) remains the cornerstone of rhythm evaluation. In arrhythmia, the ECG reveals consistent deviations: irregularly irregular R-R intervals in AF, wide QRS complexes in VT, or brief blocks in bradyarrhythmias. Dysrhythmias often show subtle abnormalities—narrow QRS complexes with brief pauses, slight repolarization changes, or transitional rhythms blending normal and abnormal features. Assisting clinician analysis are: - Holter monitoring: captures dysrhythmic episodes over 24–48 hours - Event recorders: for sporadic symptoms linked to transient dysrhythmias - Electrophysiology studies (EPS): invasive mapping for indeterminate or high-risk rhythms - Biomarkers: troponins, electrolytes, and inflammatory markers help distinguish structural damage from acute metabolic triggers Quotes from clinical guidelines underscore protocol: *“The ECG is the auditory map of arrhythmia; interpretation requires clarity on whether the rhythm is truly arrhythmic or a transient dysrhythmia borne of reversibility.”* — American Heart Association, 2023 Therapeutic Pathways: When to Act—and When to Wait Treatment diverges sharply between arrhythmia and dysrhythmia. Persistent, symptomatic arrhythmias typically demand definitive therapy—anticoagulation for stroke prevention in AF, beta-blockers for rate control, or ablation for rhythm restoration. Dysrhythmias, often due to modifiable causes, warrant addressing the root: correcting dehydration, adjusting medications, or treatingHypokalemia or hypomagnesemia. Yet not all dysrhythmias need direct intervention—some self-terminate after correcting sodium levels or stopping a sedative. In contrast, recurrent sustained VT or unstable VT profiles mandate urgent implantation of cardiac defibrillators or advanced heart failure therapies, as they carry high risk of sudden cardiac death. A 2022 meta-analysis in *Circulation Research* emphasized this: “Distinguishing arrhythmia from dysrhythmia prevents both under-treatment of life-threatening rhythm disorders and over-treatment of transient electrical noise.” Real-World Challenges: The Ambiguity in the Signal Ambiguity often lies in the “gray zone” where dysrhythmias mimic arrhythmias. Atrial fibrillation with irregular wide QRS complexes can appear as combined pathology. Posterior wall infarcts may produce non-sustained VT with unstable morphology. Clinicians must avoid mislabeling transient dysrhythmias as fixed arrhythmias—misdiagnosis risks inappropriate ablation or overused antiarrhythmics. < They are not isolated events but signsposters of deeper cardiac distress. Dysrhythmias, though transient, act as early warnings—cues demanding proactive evaluation before progression. Whether a heartbeat races too fast or skips a beat unexpectedly, the distinction guides precise, patient-centered care. From the lab bench to the ER floor, clarity between arrhythmia and dysrhythmia empowers clinicians to distinguish between benign fluctuations and urgent threats, ensuring no heartbeat is ignored—and no risk is left untraced. In the race against cardiac inefficiency, recognizing this difference is not just anatomically important—it’s life-saving.


Related Post
Rubbing Hands Together Meme: How a Simple Gesture Defined a Global Emotion During Crisis
:max_bytes(150000):strip_icc()/1960s-couple-man-woman-men----563966211-5a63b2c4482c520037cbc1ef.jpg)
When Color TV Was Invented: The Decades-Long Journey Behind America’s Visual Revolution

Ashley And Ryan Eldridge’s New House: A Dream Home Built on Craftsmanship, Comfort, and Contemporary Vision

Kim Reeves: A Deep Dive Into the Life and Legacy of Keanu Reeves’ Sister