And Pseudoephedrine: The Dual-Faced Medicinal Powerhouse With a Shadow of Regulation
And Pseudoephedrine: The Dual-Faced Medicinal Powerhouse With a Shadow of Regulation
Pseudoephedrine, a compound long recognized in pharmaceuticals for its decongestant efficacy, sits at a crossroads of medical necessity and regulatory scrutiny—largely due to its role as a key precursor in illicit methamphetamine synthesis. Found in over-the-counter cold and allergy medications, it acts as a stimulant by constricting nasal blood vessels, reducing swelling and congestion. Yet its chemical versatility makes it a target for illicit manufacture, prompting stringent oversight.
Understanding pseudoephedrine’s impact demands a precise look at its pharmacology, medical applications, and the complex balance between public health and security.
Chemically classified as an amphetamine derivative, pseudoephedrine (C₁₀H₁₅NO) is structurally related to ephedrine but differs in its configuration, conferring selective activity at nasal decongestant receptors. When ingested, it crosses the blood-brain barrier slowly, exerting mild central nervous system stimulation but primarily peripheral action.
Unlike methylphenidate or amphetamine, it produces minimal euphoria, reducing its abuse liability but not eliminating potential misuse—especially in clandestine labs where it is extracted from over-the-counter products. Only compounds pulverized from products containing concentrated pseudoephedrine can yield illicit stimulants, according to the U.S. Drug Enforcement Administration (DEA), making its presence in OTC formulations a dual-edged sword.
In clinical settings, pseudoephedrine remains a cornerstone therapy for nasal congestion caused by colds, sinusitis, and allergies. The National Center for Biotechnology Information (NCBI) notes its efficacy in reducing edema in nasal mucous membranes, offering relief within 20 to 30 minutes and lasting up to 12 hours when dosed appropriately. Available in tablets, syrups, and nasal sprays, it is frequently paired with antihistamines or decongestants like phenylephrine, though recent guidelines advise caution with prolonged use—exceeding three to four days—to avoid rebound congestion, a condition known as rhinitis medicamentosa.
Long-term safety studies show minimal systemic absorption when used as directed, yet patients with hypertension or cardiovascular conditions remain at risk for elevated blood pressure and heart rate.
Despite its therapeutic benefits, pseudoephedrine’s role in the illicit synthesis of methamphetamine has cemented its status as a controlled substance across most jurisdictions. The Substance Abuse and Mental Health Services Administration (SAMHSA) reports that meth labs—often small-scale and clandestine—routinely extract pseudoephedrine from cold medications, with thousands of seizures annually.
This has driven global regulatory measures: in the United States, the Combat Methamphetamine Epidemic Act of 2006 imposed daily purchase limits and mandatory ID checks, reducing non-medical access while preserving patient access. Similar controls exist in Australia, Canada, and the European Union, where pharmacies screen bulk purchases and maintain deterrent inventories.
But the story doesn’t end with control—pseudoephedrine’s utility extends beyond cold remedies.
In veterinary medicine, it is occasionally used to treat nasal congestion in larger animals, though formulations differ due to species-specific metabolism. Veterinary formulary updates caution against human misuse in animal products, reinforcing the compound’s pharmacological boundaries. Meanwhile, in drug development, pseudoephedrine continues to inform the design of safer decongestants, with researchers seeking analogs that maximize nasal vasoconstriction while minimizing CNS stimulation and abuse potential.
Enforcement and medical communities remain locked in an ongoing effort to preserve pseudoephedrine’s therapeutic value while curbing its diversion. The DEA emphasizes that legal access hinges on strict compliance with anti-diversion protocols: only authorized distributors may stock high-risk OTC products, and serial numbers are recorded to trace back to retail sources. Pharmacies deploy automated dispensing systems that deny excessive fills, and public awareness campaigns highlight responsible use.
These measures aim not to eliminate access but to make misuse exponentially harder—reducing diversion without compromising patient care.
In high-stakes pharmacology, few compounds embody this tension quite like pseudoephedrine. Balancing relief against risk, science with regulation, and medical need with public safety defines its legacy.
Every tablet dispensed, every policy adjusted, reflects a calculated effort to harness a powerful molecule’s benefits while halting its journey into illicit hands—proving that even life-improving drugs require vigilance, innovation, and shared responsibility.




Related Post

78.3 Kilograms to Pounds: The Definitive Conversion From Metric to Imperial

Kaitlin Collins: The Unseen Force Behind a Growing Boyfriend Presence
Unlocking the Power of Radicul O: The Secret to Faster Neural Learning
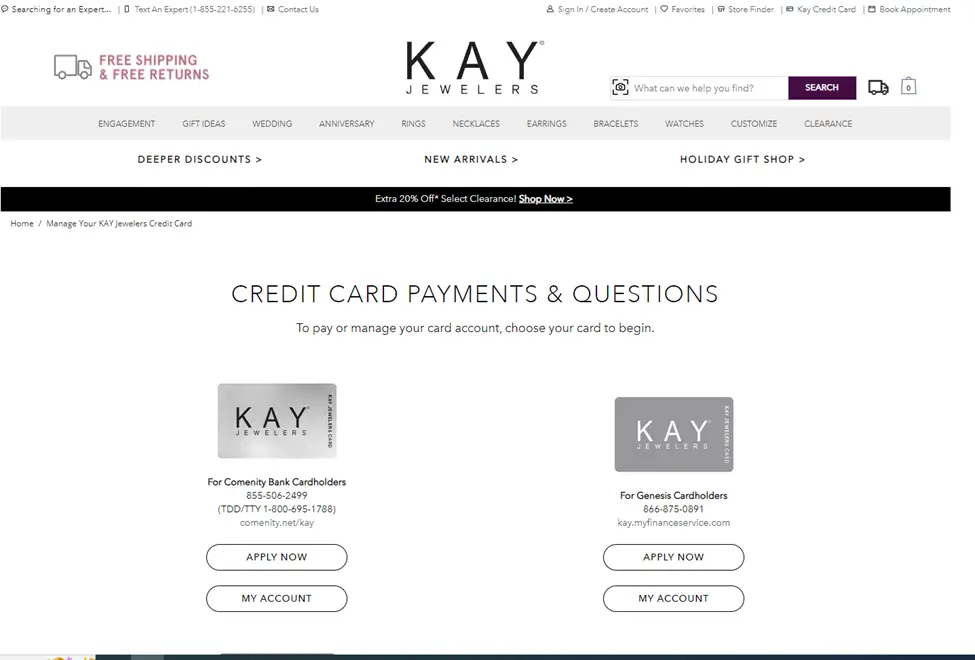
Kay Credit Card Login: Secure Access, Seamless Financial Management

